The therapies are being developed in Toronto General Hospital Research Institute’s (TGHRI) Latner Thoracic Surgery Research Laboratories drug discovery and delivery pipeline. Involving more than 100 personnel, the research team collaborates on lung injury, transplant, regenerative medicine and thoracic cancer studies.
More than 80 per cent of potential donor lungs are injured and show inflammation due to the process of brain or cardiac death and intensive care-related complications, and cannot be used for transplantation. Infection and organ rejection are the two main complications after transplant surgery.
The goal of the two therapies is to prevent acute lung injury during surgery and reduce post-operative complication, leading to better survival outcomes and quality of life for patients.
Transplanting lungs that function better from the start would lead to more predictable, safer outcomes, shorter periods of mechanical ventilation, and shorter stays for patients in the intensive care unit.
The IL-10 gene plays a role in inhibiting the immune response to inflammation or foreign materials, such as transplanted organs. The other therapy, an Alpha-1 antitrypsin (A1AT) drug, used for emphysema patients, can reduce inflammation and cell death during transplantation.
Both IL-10 gene therapy and A1AT are expected to begin clinical testing at UHN as early as 2018.
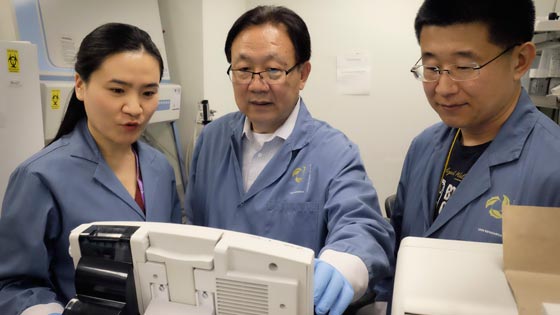
“Through new drugs researched within this pipeline, we are helping patients get a better surgical outcome,” said Dr. Mingyao Liu, co-founder of Latner Labs, Senior Scientist at TGHRI, Director, Institute of Medical Science and Professor of Surgery, Faculty of Medicine, University of Toronto.
“Our advances can improve the quality of the donor lung by decreasing inflammation and repairing injured lungs so that the transplanted organs function better from the beginning.”
“Everything we can do to prevent lung injury, especially in the first 72 critical hours after surgery, would have a significant impact on survival and quality of life after transplantation,” said Dr. Shaf Keshavjee, Director and co-founder of Latner Labs, Director of the Toronto Lung Transplant Program, and UHN Surgeon-in-Chief. He adds that patients who have severe early lung injury are at greater risk of dying after surgery, and have higher rates of organ rejection later on.
The incidence of primary graft dysfunction—a post-operative condition that leads to early morbidity and mortality in lung transplant recipients—is 10 to 25 per cent. Five-year survival rates worldwide for transplant patients are about 50 per cent—well behind those of other solid organ transplants.
Old therapies made new
IL-10 gene therapy works by counterbalancing inflammatory mediators before and during transplantation.
To overcome some of the challenges of gene therapy, the researchers first developed a strategy to preserve lungs at normal body temperature, with the lungs kept outside the body in a protective sterile dome.
The Toronto Ex Vivo Lung Perfusion System (EVLP) —a world-first technique developed by Dr. Keshavjee in 2008—continuously pumps a bloodless solution, proteins and nutrients into injured donor lungs, mimicking normal physiological conditions. This makes it possible for injured cells to begin repairing themselves and sets the stage to apply more sophisticated repair techniques to donor lungs.
Then, using a specially engineered adenovirus vector—a common cold virus—the researchers used a bronchoscope to inject the vector with an added IL-10 gene through the windpipe into human lungs during EVLP. The vector carries the IL-10 gene into the tissue cells, activating the mass production of encoded IL-10 cytokines—proteins that inhibit the function of pro-inflammatory cytokines.
Through triggering IL-10 cytokine production, gene therapy can protect tissue from damage caused by reperfusion injury—an inflammatory response when blood and oxygen are reintroduced into the organ once it has been inserted into the recipient’s body.
Dr. Keshavjee said the frontier of lung transplant research is repairing and modifying donor lungs to be better than the state it was received in for surgery.
“That’s a fundamental shift in the way people thought about transplant,” Dr. Keshavjee said. “It was always about getting the organ, trying to preserve it as it slowly deteriorates. Now, we can get the organ to get better over time.”
“That was something we thought about 15 years ago – but now we’re there.”